Updated: 15 August, 2024
The field of healthcare is constantly evolving. New medical advancements emerge at an unprecedented pace, demanding healthcare professionals to be lifelong learners.
There are hundreds of different elements involved in the training of healthcare which contribute to a student’s learning.
Throughout this blog we will take a look at what reflective practice is, the importance of reflective practice in healthcare, a framework for reflective practice, and how our tool Videolab is a perfect solution for self reflection.
Key takeaways:
- Reflective practice fuels ongoing professional development in healthcare, fostering adaptability and growth in response to evolving medical landscapes.
- Frameworks like Gibbs Reflective Cycle and Kolb’s Cycle provide systematic approaches for insightful reflection, guiding professionals to identify areas for improvement and drive continuous growth in practice.
- Delayed feedback promotes deeper reflection, boosts retention, and enhances learning outcomes.
- Videolab is a powerful innovative tool which offers offers a dynamic platform for self-reflection and collaborative feedback, enhancing communication skills and preparing students for real-world practice.
What is Reflective Practice in Healthcare?
Reflective practice is the process of critically analysing and evaluating your experiences, actions, and decisions to gain insights, enhance learning and improve for future practice. It’s essentially taking a step back after an encounter with a patient, a challenging situation, or even a success story to think deeply about what happened.
The analysis goes beyond just facts and explores feelings, actions, outcomes and more. Questions are asked such as:
- Did you feel confident, unsure, or overwhelmed at any point?
- What did you do and why?
- Were there alternative approaches that could have been taken?
- What was the result of your actions?
- What could have been done differently to achieve a better outcome?
- (if applicable, e.g during a consultation) do you think your patient felt comfortable, did you clear any questions they had, did you communicate the situation to the best of your ability?
Reflective practice is so important as it empowers professionals to continuously learn and improve, ultimately enhancing the well-being of individuals and communities. Through reflection, practitioners gain valuable self-awareness, allowing them to identify areas for growth and adapt their care delivery methods. This translates to better patient experiences and outcomes.
The benefits extend beyond individual practice. Consistent reflection fosters stronger multidisciplinary teams. By critically analysing experiences, professionals can identify opportunities to decrease reliance on any single team member and empower individuals receiving care. This collaborative approach leads to greater independence for patients, giving them more control and choice in how their care is delivered (The Access Group).
Read this blog to learn more about shared decision making from an expert in the field.
Why is reflection important in training?

Self reflection is a crucial part of medical education. Not only in the practice and learning of healthcare, but also as a daily practice throughout your career. Medicine is always changing, new challenges arise, and many new treatments and breakthroughs happen every year. Therefore, healthcare professionals must be constantly learning and growing. Self-reflection instils a habit of critical thinking and self-evaluation, promoting a lifelong commitment to learning and staying current with advancements.
In addition to this, the importance of reflective practice helps trainees make better decisions. It allows trainees to connect past experiences with current situations. This deeper understanding allows them to make more informed and effective decisions in the future.
Through reflection, medical trainees gain a deeper understanding of their strengths, weaknesses, biases, and emotional triggers. This self-awareness allows them to identify areas for personal and professional development.
Moreover, reflecting on patient interactions allows trainees to consider the patient’s perspective and understand their emotions. This fosters empathy and compassion, a critical skill for building trust with your patients and their family.
Studies
A paper written in the National Library of Medicine highlights the importance of reflective practice in medicine. The paper assessed 477 residents and fellows in 16 different studies and concluded that “Reflection increased learning of complex subjects and deepened professional values. It appears to be an effective tool for improving attitudes and comfort when exploring difficult material.”
Another paper from the Health and Care Professions Council, highlights how reflective practice can contribute to self-awareness as one of its key benefits. By critically analysing experiences, both positive and negative, healthcare professionals can gain insights into their strengths and weaknesses. This self-awareness allows them to identify areas for improvement and ultimately deliver better care. The paper emphasises that reflection is a continuous process, not a one-time event.
Self-reflection also provides a powerful tool for medical professionals to develop their emotional intelligence. By reflecting on their own emotions in challenging situations, medical professionals can identify triggers and develop coping mechanisms. This self-awareness allows them to manage their reactions and improve communication with patients and colleagues. By gaining a deeper understanding of their own emotions and those of others, they can build stronger relationships, ultimately leading to better patient care and improved well-being for both parties.
Developing Reflective Skills
Reflective practice isn’t a passive process; it requires active engagement and practised skills.
According to the National Library of Medicine one of the models for self reflection is going through the stages of reflecting. Understanding the “why” behind each stage empowers trainees to gain deeper insights from their experiences.
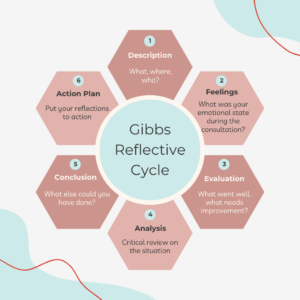
These stages were designed by Graham Gibbs in 1988, now commonly referred to as Gibbs Reflective Cycle. It is a guide for structured reflection. This popular model guides you through a structured process of analysing your experiences in any situation. It is widely used in fields such as healthcare and education. A survey from the British Journal of Midwifery found that 63% of healthcare professionals regularly used Gibbs Reflective Cycle as a tool for reflection (source).
The cycle itself is a roadmap with six distinct stages. By working through each stage, you ensure your reflection has a clear purpose and leads to actionable insights. Ultimately, the Gibbs Cycle encourages you to delve deeper into your experiences, identify areas for improvement, and refine your practice for the future.
Gibbs Reflective Cycle
The six stages are as follows:
Stage 1: Set the scene.
Start by asking “What, where, and who?” Describe the situation in detail: what happened, where were you, and who was involved? Reflect on your role and the overall outcome.
Stage 2: How did it make you feel?
Delve into your emotional state. What were your thoughts and feelings during the experience? Honesty is key. Were you scared, confused, or perhaps frustrated? Understanding your emotions helps you connect them to the situation and identify potential triggers for the future.
Stage 3: Why did it happen?
Make sense of the situation. Analyse the interaction of yourself, the situation, and others involved. Think about why things happened as they did. Did things go smoothly, or could there have been improvements?
Stage 4: Learning from hindsight
Critical review of how the situation went and if you could rewind and approach the situation differently, would you? Identify factors you could have influenced and consider alternative approaches that might have led to a better outcome.
Stage 5: What will you do differently in the future?
This is arguably the most important stage in reflecting. Take all your learnings and translate them into actionable steps for future encounters. Don’t limit yourself to the specific situation; consider transferable skills and knowledge that might apply elsewhere.
Stage 6: Putting your learning to the test
Test your reflections. As you encounter similar situations, observe if your approach aligns with your reflections. This continuous “test and refine” cycle strengthens your understanding and ultimately improves your practice.
By following these steps and actively engaging in reflection, you’ll unlock a powerful tool for growth and continuous learning. Reflection empowers trainees to become a well-rounded healthcare professional, delivering the best possible care to patients.
Trainees should also constantly seek feedback from supervisors and peers to gain different perspectives and help keep an open mind throughout the evaluation process. By incorporating this external feedback, trainees can gain a more well-rounded understanding of the situation and ensure their evaluation is comprehensive and objective.
Kolb’s Cycle of Reflective Practice
Another reflective framework is Kolb’s Cycle of Reflective Practice, developed by David A. Kolb, the cycle consists of four stages. Concrete Experience, Reflective Observation, Abstract Conceptualisation, and Active Experimentation. This framework provides a structured framework for individuals to engage in continuous learning and improvement by systematically reflecting on experiences, gaining insights and applying them in practical contexts. This cyclical process fosters deeper understanding, skill development, and professional growth in various fields, including healthcare.
Stage 1: Concrete Experience
Where trainees engage in hands-on experiences or real-life situations. This stage involves direct involvement in an activity, such as participating in a clinical scenario during healthcare training.
Stage 2: Reflective Observation
Trainees should step back from the experience to reflect on what happened, considering their thoughts, feelings, and reactions. Thinking about how the experience links to your skills, knowledge and prior experience.
Stage 3: Abstract Conceptualisation
Where trainees make sense of their experiences by analysing them and drawing conclusions. In the context of healthcare training, this stage involves identifying patterns, principles, or theoretical frameworks that explain the observed outcomes or behaviours.
Stage 4: Active Experimentation
This is where trainees apply their newfound insights and understanding to real-world situations. Trainees should ensure any goals set are specific, measurable, achievable, realistic, and targeted.
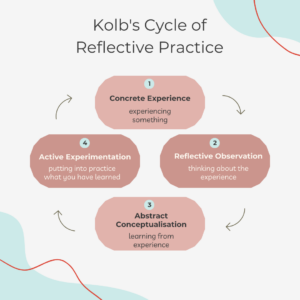
As you can see, both frameworks share similarities in their fundamental concepts and objectives, but they differ in their structures and emphasis. Both models aim to guide trainees through a process of reflection to facilitate learning and personal development. Kolb’s Cycle consists of four stages which focus on the holistic learning process, starting with direct experience and progression through reflection and application. On the other hand, the Gibbs Reflective Cycle has six stages. This model provides a more detailed framework for reflection, with specific emphasis on exploring feelings and evaluating experiences before drawing conclusions and planning actions. While both models serve as valuable tools for reflective practice, individuals may find one model more suitable than the other depending on their preferences, learning styles, and specific contexts.
How to practise self reflection
An effective method to learn reflective practice is through simulation exercises, where trainees engage in realistic scenarios mirroring clinical situations. After these simulations take place, typically debriefing sessions come into play and serve as a crucial platform for reflection.
Should reflection take place immediately after the consultation or delayed?
A study by J. Williams (2012) showed that delayed feedback is more beneficial than immediate feedback due to several reasons:
- Enhanced reflection: Delayed feedback allows learners more time to reflect on their performance and experiences. This extended period of reflection encourages deeper analysis and understanding of the situation, leading to more profound learning outcomes.
- Increased retention: When feedback is provided immediately after an activity, learners may focus solely on the feedback itself rather than the experience. However, with delayed feedback, learners have the opportunity to internalise the experience before receiving feedback, leading to better retention of the feedback and its associated lessons.
- Facilitation of metacognitive skills: Delayed feedback promotes the development of metacognitive skills, such as goal-setting and monitoring progress. By allowing learners to reflect on their performance over time, delayed feedback supports the development of strategies for self-regulated learning, ultimately leading to more effective skill development and knowledge acquisition.
Overall, the study suggests that delayed feedback provides learners with valuable opportunities for reflection, self-assessment, and metacognitive skill development, leading to more meaningful learning experiences and improved performance outcomes.
This is where Videolab comes in…
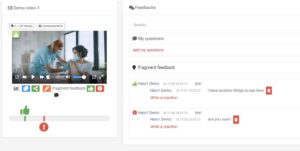
Videolab is an innovative video-based feedback platform, revolutionising the learning experience by enabling students to share consultations with professors or peers, facilitating valuable feedback and self-reflection.
By enabling students to record and share patient or simulation consultations in a safe environment, Videolab promotes a reflective learning approach. Students are able to look back on the recording and review their own performance, identify areas for improvement. They are able to engage in self-reflection through the time-fragmented feedback feature which allows them to timestamp moments in consultation where they believe they either performed well, need improvement, or would like to assign a question for their assessors opinion.
These recordings are then shared with pre approved assessors to mark and evaluate. The secure collaboration tool also allows trainees to securely share the recording with peers and receive feedback from multiple different sources.
Videolab has become the go-to tool for doctor patient communication training and consultation training in the Netherlands and is slowly increasing its use cases nationwide.
Conclusion
This blog has highlighted the vital role of reflective practice in healthcare training, underscoring its significance in nurturing lifelong learning and elevating patient care.
Reflective practice, as explored, is not merely a passive exercise but an active process of critical analysis and evaluation. It empowers healthcare practitioners to delve into their experiences, emotions, and actions, fostering self-awareness and continuous improvement. Through structured frameworks like the Gibbs Reflective Cycle and Kolb’s Cycle of Reflective Practice, professionals gain a roadmap for insightful reflection, leading to actionable insights and refined practices.
Furthermore, the incorporation of delayed feedback, helps trainees gain thoughtful reflection and enable deeper analysis, and professional growth.
Innovative tools such as Videolab transform learning experiences. Enabling students to record and reflect on consultations, Videolab facilities self-assessment and collaborative feedback, paving the way for enhanced doctor-patient communication and consultation skills.
