Updated: 17 May, 2024
The Dutch population is blessed with an excellent healthcare system. The Netherlands has a consistent place in the top three of the world index of healthcare innovation and scores highly on many other medical quality indexes. Anyone working in quality knows that quality is a process not a destination. In a series of interviews I talked to some of the people who work hard every day to deliver this quality. The educators who train tomorrow’s doctors.
One of the first things I learned in these conversations is that the current big leap in the quality of healthcare is all about the psychological and the human side of care. Gone is the arrogant doctor who makes you feel uncomfortable and inadequate. The Dutch training institutes are championing topics such as doctor patient communication training, patient centered care and joint decision making. Communication training plays a much bigger role in the formation of doctors.
So we should expect tomorrow’s doctors to be much better at listening, much better at guiding the conversation towards what really matters and much better at explaining things in a way we can understand. We know that this will lead to better health outcomes either directly or indirectly via psychological or behavioral factors. But how exactly are doctor patient communication skills learned?

Key Takaways
- Interactions with patients are recorded.
- Feedback can be given by trainers, experts but also peers.
- The adequate device for recording depends on the context, it may a fixed camera, a tablet or event the trainees phone.
- Trainees are sometimes reluctant to get started with recording, but are very positive when reflecting on the learning experience.
How the University of Maastricht trains consultation skills.
At the University of Maastricht I interviewed Monique Kentstra who is the Videolab coordinator of the skillslab and Dr. Ramona Guerrieri, coordinator of the GP training program.
How consultation skills are trained at the skillslab
At the skillslab they work a lot with simulation patients. The simulation patients are trained by the university and each one plays a specific role. For the bachelor in healthcare there are 7 scenarios per year over 4 years. So in total there are 28 scenarios played out by actors at the skillslab for the bachelor training. They also train medical researchers with this methodology.
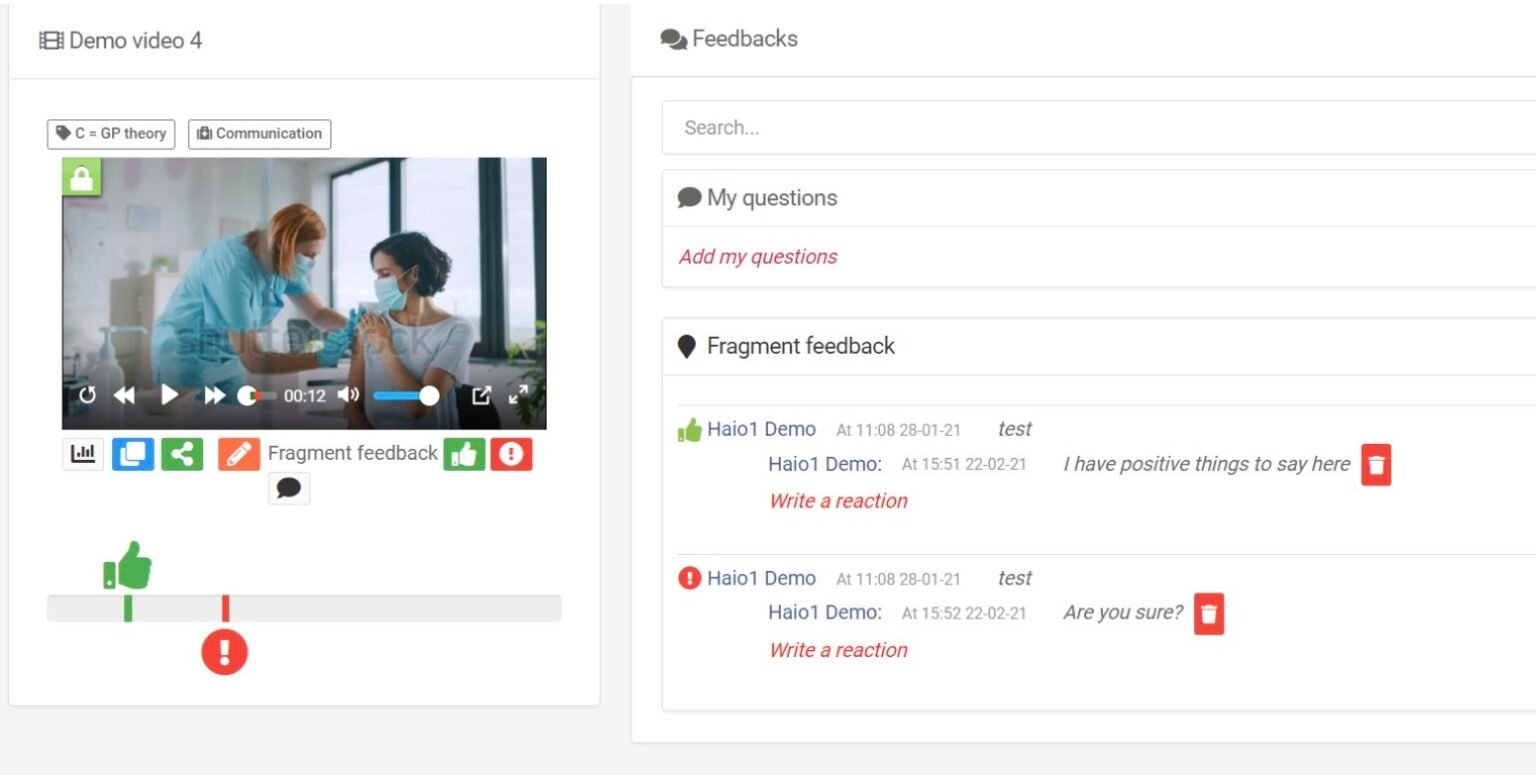
Trainings are recorded using Cloudcontrol and Videolab. The recordings are used in the first instance for peer feedback, students give each other feedback on the scenario played out. The instructor sees all the comments, but the peers don’t see each other’s comments. This is done so that each has come up with their own feedback on the interaction. The trainee on the video receives everyone’s feedback.
Additionally, per trainee, there is top down evaluation of at least three simulation recordings per year. These may be accompanied with coaching conversations between the trainer and the student.
Students can also train independently by recording sessions with the simulation equipment such as simulation mannequins, for medical skills, or roles played among trainees for communication skills. These recordings are used in the first place for self reflection but trainees can also use Videolab to safely share with others and voluntarily request feedback.
The recordings of simulations are also used to provide feedback to the simulation actors to help them improve on their performance.
Monique tells me that they are currently working on similar Videolab training methodologies for the master students but then with real patients instead of simulation patients. They hope to roll these out in the coming semesters.
As a camera setup they use a fixed camera setup integrated with CloudControl. For the independent training, students use their own devices with the Videolab app.

How communication skills are trained in the GP program.
GPs in training often do their residency at different local clinics, Ramona tells me. In these clinics there are often fixed camera setups that are used to record the communications between doctor and patients. Cameras are set up so that both the faces of the doctor and the patient are visible.
Some of the topics trained in the GP training program are: empathy, establishing connection, exploring and distilling the care request, and joint decision making. Doctor patient communication training is evaluated using the MAAS2.0 evalution method. MAAS is a standardised evaluation methodology used across the Netherlands, especially but not exclusively in GP training.
In the GP training program they also use Videolab to train the trainers. Interactions between trainer and trainee are recorded. Other trainers review the interaction and provide feedback.
In this field of training methodologies for GP trainers Dr. Angelique Timmerman did some interesting research at the university of Maastricht. She looked at the different behavioral profiles of the trainees. Their performance is measured on two dimensions: 1: Clinical expertise and 2: Doctor patient communication. This leads to 4 typologies of performance in GP trainees and, most usefully, specific guidelines for coaching each typology. Her paper can be found on researchgate here.
Practical learning as GP is often done in groups where trainees give each other feedback as well as self-reflect upon their recordings. Here fragment feedback is used a lot. Later on these skills will be evaluated by a different trainer that has no prior relationship with the trainee to objectively establish that the learning outcomes are achieved. For this, in Maastricht they evaluate 6 consultations of each trainee with the MAAS2.0 method.
Ramona mentioned that having a doctor in the room, supervising a trainee in his or her conversation with the patient, actually has an influence on the dynamic of the conversation. The patient does not ignore the second, more senior doctor and may start addressing her in the conversation. It is therefore better to record the conversation and let it flow naturally.
These conversations can then later be watched together with the more senior doctor that is providing guidance. “Seeing yourself recorded is very powerful for self reflection” Ramona points out. And the trainer will be there at that moment to help analyse and internalise the learnings.
How the Odontology School of University Medical Center of Groningen trains communication skills.
At the dental school of UMCG I spoke to Aline Goldshmidt, lecturer in communication training.
Aline told me that there are 5 compulsory recordings trainees have to make that cover essential aspects of the communication training. These are gathered as a portfolio demonstrating communication skills. There are two in the bachelor which are done with a fellow student in the role of the patient and three in the masters with real patients.
The first conversation in the bachelor training is the intake conversation. This is the first conversation the doctor has with the patient in which he or she is to explore the complaint, the history, etc… Here a fellow student will play the role of the patient.
The second conversation in the bachelor training is the Behavioral Change conversation. In this training students are encouraged to broaden the scope to any real behavioral change students may be aspiring to. Hence the conversation becomes about that behavior and it is more realistic. Students give each other peer feedback on the recordings.
The third conversation which takes place in the master is the first one with a real patient. This conversation is the treatment plan discussion. Aline explicitly mentioned the importance of reading non verbal communication in this interaction. Is the patient still following? Does he understand what I am saying? The interaction is recorded and the trainee reviews the interaction for self reflection and then shares it together with his fragment annotations with a trainer for feedback.
The fourth and fifth conversations are either Fear Conversation, Motivational Conversation or Bad News Conversations. The trainee chooses two of these to submit in their second and third year of the master.
The fear conversation is the hardest one to record because patients that are afraid are per definition not feeling very comfortable and the least happy about being filmed. Consent to be recorded is voluntary of course, so if the patient does not agree the dentist will have to wait for another opportunity to present itself. Aline points out that a lot depends on how consent is asked, she advises to first establish a relationship with the patient, build some rapport and trust. After that it is easier to request consent for recording.
In the bad news conversation the patient will be informed of something negative, something that may impact his or her quality of life going forward. Bringing bad news is no easy task. As a caregiver you want to be clear but not blunt. Notice that the most emotionally charged conversations are trained later in the training as these require more mature communication skills.
On a practical level the dental clinic provides the handheld cameras that are used for recording. They experimented with fixed cameras but saw better results with handheld cameras. They try to set up the camera so that both the patient and the dentist are in the frame.
Communication training at the ETZ hospital
At the ETZ hospital I spoke to Jan van den Eertwegh en Jack Van De Langenberg who are both responsible for communication training at the hospital.
Jack and Jan tell me that video recordings are used at a wide range of specialties in the hospital. For psychology and neurology this is currently a fundamental component of the training. For others, such as, internal medicine, pediatrics, neurosurgery there are voluntary learning cycles with recordings focussed on developing communication skills. Others, including radiology, are considering starting with the methodology.
At ETZ cameras are set up for one specific part of the day and during this timeframe as many patient interactions as possible are recorded. This is off course, as always, subject to patient consent. These recordings are then reviewed by communication experts, such as Jack, who provide feedback to the doctors. ETZ relies on a pool of specific communication specialists.
As the use here is voluntary for the trainee, in many cases, they saw some reluctance to record themselves. “Nobody likes to see themselves on camera”. But in retrospection, all the doctors that participated found the exercise useful, learned a lot, and would recommend it for other doctors.
Picking up on this Jack and Jan decided to make a video about the hesitations and experience of these doctors. Basically doctors sharing their positive experience with the program, to convince more doctors to voluntarily participate.
At ETZ they use an adaptation of the MAAS 2.0 that is designed to include more topics related to joint decision making. This training is always formative and students do not get “graded”. However they can get a certificate of completion.
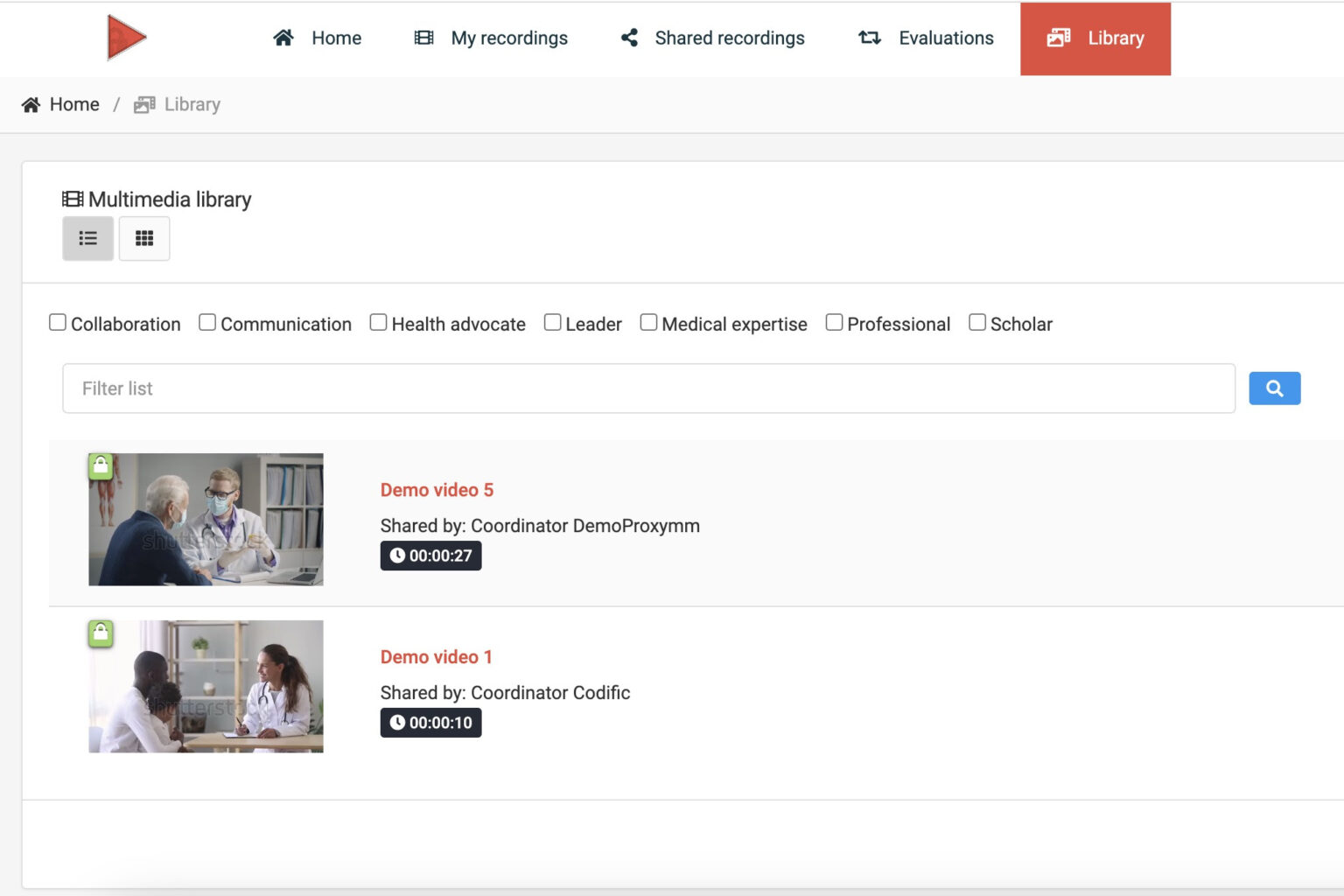
Nurses are also trained using these video feedback methodologies. Additional attention is paid to EPAs, Entrustable Professional Activities. With this, competence based decisions can be made on the level of supervision required by trainees. The CanMEDS competencies are integrated as labels in Videolab, that way videos can easily be categorized, grouped and found based on the CanMED competency they cover.
At the time of this writing ETZ is preparing new recording based training programs for inter professional collaboration. Here they will record interactions between specialists and to develop a new evaluation to provide feedback in these interactions.
This summer the Codific team attended the conference of the International Association for Medical Education (AMEE). This edition in Glasgow was focused on multi disciplinary collaboration. This seems to be a topic of growing importance and it is great to see ETZ lead the way. We also noticed the IPSIG-week in Antwerp where a wide range of Dutch and Belgian healthcare trainees come together for a week to train interdisciplinary collaboration. Fun fact, the IPSIG week uses Codific’s Attendance Radar to track the attendance of 900 students across 55 events.

From a practical perspective doctors use their own smartphones to record with the Videolab app. They found this to work better than providing and keeping track of different devices by the hospital. The special Videolab recorder app makes it possible to securely record patient interactions with a private smartphone. Simple tripods are used to set up the phone and they try to have both doctor and the patient in the shot. Jack also mentioned that additional attention is paid to not putting the phone too far away as the default microphone of a smartphone is not good at picking up sound from further away.
Conclusions
These are just a few of the many educators who train tomorrow’s doctors in the Netherlands. Many others provided feedback about their methodologies upon my request, and I hereby explicitly would like to thank all the people who contributed, everyone was very generous with their time and insights. I do believe that the stories narrated here are quite representative of the scope across Dutch healthcare education. These interviews were done in the fall of 2023 and everyone had big plans for the future. This article will be quickly outdated, and that is great to see. Quality and innovation are an essential component of the Dutch educational culture leading to organizations that are continuously moving forward, learning from the present to teach better in the future.
If you are involved in communication training for healthcare professionals and have a story to share, or if you feel like there is something I misunderstood please don’t hesitate to reach out to me below.
