Updated: 25 January, 2024
What is shared decision-making in healthcare?
Shared decision-making (SDM) in healthcare is a process in which healthcare providers and patients work together to make decisions about the patient’s care. This means that the patient is not simply told what to do, but is instead involved in the decision-making process. SDM is important because it can help to ensure that patients receive the care that is best for them, given their individual circumstances and preferences.
SDM is founded upon the principle that patients have the right to participate actively in their healthcare decisions. It is also based on the evidence that SDM can lead to better patient outcomes, including increased satisfaction with care, improved adherence to treatment plans, and reduced decisional regret.
A conversation with shared decision making expert, Haske Van Veenendaal
I had the privilege of speaking to a very highly respected expert in the field of shared decision making, Dr. Haske Van Veenendaal. Haske is a researcher and PhD graduate at the Erasmus School of Health & Policy Management, a member of the supervisory board of Mytylschool Gabriel and the owner of an academy which provides shared decision making training, Trant – for the Care of Tomorrow.
His expertise in shared decision-making is extremely interesting, drawing from his extensive experience and profound grasp of the field’s theories, methods, and procedures used in practice.
If you would like to learn more about how shared decision making is taught, its teaching methods, challenges in the field and related topics, listen to the podcast linked below.
A transcript is also available at the bottom of this page.
Additionally, you can find the video podcast on our Youtube linked here.
The information below is based on the insights gained from the interview and other research conducted. All sources cited.
Why is shared decision making in healthcare important?
From research, we can gather that shared decision making in healthcare is very important based on the fact it improves healthcare by fostering a partnership between patients and physicians. It empowers patients to actively engage in decisions about their own health, upholding their autonomy and respecting their rights.
Shared decision making not only elevates patient satisfaction and treatment knowledge but also enhances treatment adherence, potentially leading to improved health outcomes. It is particularly invaluable when multiple treatment options exist and the optimal choice weights on individual factors such as personal preferences or coexisting conditions.
From the perspective of a professional in the field, I also wanted Haske’s opinion on why he thought shared decision making is important, and how it benefits both doctors and patients during a consultation.
He highlighted several main areas where SDM positively impacts consultations. Firstly, for the patient, having a SDM gives them autonomy over the decisions which therefore leads to less regret or upset about decisions being made.
And for doctors, introducing SDM procedures into a consultation allows for more structured conversation, and a more productive interaction with the patient.
Very interestingly enough, Haske also mentioned it also helps clinicians feel less responsible for the outcome of treatments. By sharing responsibility, the doctor can be confident that the patient has carefully considered the treatment options and is prepared for different possible outcomes.
Are there any specific frameworks or models that are used in a shared decision making consultation?
Haske meticulously outlined the general structure employed before and during a shared decision-making consultation.
Physicians first strategise for the consultation, outlining potential discussions and decisions tailored to the patient’s individual case.
From there, the doctor typically follows five steps.
- Introduction to the decision that is to be made, clearly understanding your role as the clinician, and the role of the patient during the process of joint decision making.
- Access and discuss positives and negatives of the options presented to the patient and make sure the patient fully understands what is being discussed.
- Determining what is important to the patient, what their preferences, values and priorities are throughout the procedure.
- Finding and agreeing on a decision that is supported by both the patient and clinician, taking in both the clinicians expertise in the field, and the patient’s wishes.
- The final step would be to evaluate the choices that have been made that are in line with the result both parties are wanting to achieve.
Note, Haske mentioned that this model can change depending on important factors of the patient. In practice, “it’s all about the specific context in which the clinician works”.
Doctors must deal with each case slightly differently, a cancer patient’s care is very distinct from a child’s care, such as chronic patients are from acute patients.
Doctors must have the training and ability to modify communication and behaviour of the shared decision making techniques in different contexts and healthcare settings. Training must properly prepare doctors with these skills.

Strategies to help implement shared decision making in an organisation
Haske finished his PhD this year on the “Implementation of shared decision making in daily healthcare in clinical oncology care“.
The study involved interviewing experts at a high level who already had experience in effectively implementing SDM in their practices to gather insights and recommendations for wider adoption. These professionals collaborated with 11 teams of hospitals to develop and implement multilevel SDM strategies over approximately a year.
These multilevel strategies involved the training of clinicians, looking at the organisational structure, and looking at the context in which they need to function such as the guidelines, resource allocation changes and financial influence.
The structure of implementation would need to change for each organisation type depending on the layout of the business plan.
From the research done by Haske and his colleagues, the results found that when applied properly, the multilevel implementation strategy proved to be a very effective approach to shared decision making.
6 strategies to help implement shared decision making based on National Learning Consortium, Shared Decision Making Fact Sheet. (2013)
- Invite the patient to participate: inviting patients to participate through questions allows them to voice their opinions at an early stage, helping build trust.
- Present options: patients need to be aware of the whole process that has occurred before presenting diagnosis and treatment options. Explain this process to them.
- Provide information on benefits and risks: Share impartial information from existing scientific evidence. Follow up with patients to ensure their understanding of the provided information.
- Assist patients in evaluating options: Help patients assess their options by considering their goals and concerns. Inquire about what matters most to patients and what worries them to gain insights into their preferences.
- Facilitate deliberation and decision making: Let the patients know they have time to think things over. Ask patients if there is any additional information or action they require before they can confidently make a decision.
- Support patients in implementing their decision: outline the subsequent actions they need to take. Confirm their comprehension and address any potential obstacles they may encounter while executing the decision.
How do oncology patients feel about shared decision making?
During Haske’s PhD, the researchers surveyed cancer patients to understand their experiences with SDM and their preferences in decision-making processes. They found a very interesting and surprising result. After questioning, they found that up to more than 80% of the oncology patients also wanted to discuss the option of no treatment within the diagnosis options.
Do shared decision making practices increase consultation time?
n a separate part of Haske’s PhD research, another study examined a significant barrier to shared decision making.
Shared decision-making consultations are generally perceived to require more time than consultations without SDM structure or methods.
To address this common concern, they conducted a comprehensive review of studies and found that contrary to expectations, SDM does not necessarily prolong consultations. In fact, many studies showed no significant increase in consultation duration. Twenty-eight of the 35 studies we selected did not show an increase in consultation time, suggesting that SDM can be incorporated into routine clinical practice without compromising efficiency.
Haske commented that despite evidence that SDM does not necessarily prolong consultations, there’s a lingering question about whether the initial implementation of SDM practices may temporarily increase consultation duration.
However, it’s expected that this increase would diminish as practitioners become accustomed to the new approach.
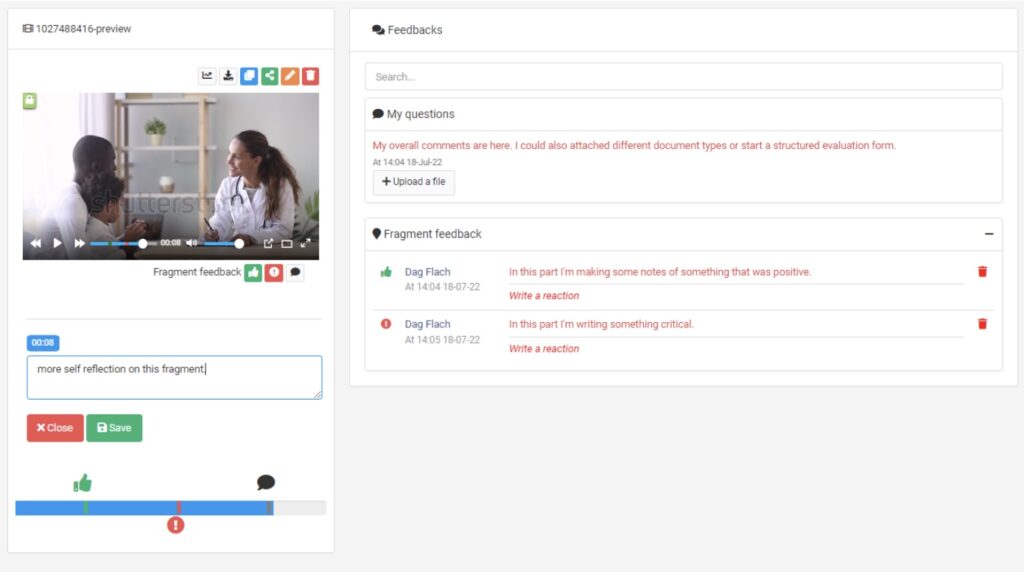
Why did Erasmus MC choose Videolab to help with shared decision making training?
Erasmus MC university was our first customer in the Netherlands, adopting Videolab in 2017, first in their GP department, then to facilitate the training of both clinical and communication skills a few years later.
So, why did they choose Videolab?
As Haske explained during the interview, The Netherlands regularly train their medical students using real patient consultations and situations.
Given the opportunity to record a series of consultations for feedback purposes and coaching provides huge value in training. Not only limiting this tool to students training, but also very much applies to helping training clinicians in an ever changing medical environment. They needed a tool which allowed them to safely record patients and to review and assess these recordings. This is where Videolab came in, providing Erasmus MC with the solution to record consultations while keeping privacy by design in front of mind, securing patient data. Also allowing students to watch back this recording in their own time, and reflect on their performance, then share with assessors for further feedback and evaluation.
Communication techniques are constantly changing, Haske recommends that clinicians should also go through consistent training to aid the practice and application of new methodologies. He believes that such a system as Videolab helps the training of communication competencies and benefits the overall healthcare environment.
Where else could Videolab be used in the future?
Videolab is already used in many places, and it has become the go-to tool for doctor patient communication training and consultation training.
As mentioned above, healthcare is constantly undergoing transformative innovations pushed by technological advancements and the growing emphasis on patient-centred care.
Haske explained two very important factors in healthcare.
The first being equality, we all have our own qualities and expertise, we also all have the right to make autonomous decisions. Patients need to feel equal in and during a consultation or healthcare procedure.
The second being, we are all unique. We must recognize our inherent differences. Clinicians must acknowledge that each patient and situation is very different.
Videolab fosters the training of a personalised approach to healthcare, ensuring that each patient receives the care they need, tailored to their specific circumstances. It’s not about adhering to rigid protocols or predetermined approaches; it’s about understanding the nuances of each individual and tailoring care accordingly.
Read the full transcript
Michaella Masters
OK, brilliant. So, hello, everyone. I'm Michaella. I'm a growth strategist at CODIFIC where I work in sales, SEO efforts and marketing efforts. Over the past couple of years, I've been doing interviews with healthcare professionals all over Europe about Videolab and its use cases. So, I've actually seen your name pop up many different times.
It's a pleasure to have you here with us today. And for the audience, we're here with Haske Van Veenendaal. I'm really sorry if I completely butchered your name.
Haske Van Veenendaal
It was pretty close. Yeah.
Michaella Masters
Okay, that's good. So if you could please go ahead and introduce yourself for the audience.
Haske Van Veenendaal
Yes, of course. Well, my name is Haske Van Veenendaal, to pronounce it in Dutch, and I'm a health scientist. I studied health sciences at the University of Maastricht, and I specialized in healthcare quality. And within healthcare quality, I further specialized in patient perspective and shared decision making. And I've been working within patient organizations, within hospitals, within, how you call it, academic institutions that focus on health care improvement. And last seven years, I've also done a PhD project or finished a PhD project on shared decision making in oncology care.
Michaella Masters
Brilliant. And also I saw that you were also an owner of a business that provides shared decision making training.
Sorry, my voice is cracking because I'm a little bit ill. Sorry, I don't want to say the name because I think I'm going to pronounce it terribly, but could you tell us a little bit about that?
Haske Van Veenendaal
Well, I have my own business, and that's called Tront for the Care of Tomorrow. So it's about how to improve healthcare. But I've already set up another organization, a network business in which we gather as trainers for shared decision making. It's called the School for Shared Decision making in English, then in Dutch, it's different. And we're giving a lot of presentations, doing a lot of training, and we also work with, how do you call it, collecting consultations via the CODIFIC system. So we have different training forms and we work a lot with healthcare professionals in the Netherlands.
Michaella Masters
Brilliant. And just to kind of take a step back, how did you get involved with shared decision making?
Haske Van Veenendaal
Yeah, that's already about 16 years ago, and in that time, we were thinking a lot about how to better involve patients in healthcare quality improvement and, for example, in guideline development or audits that were performed in hospitals. And at that time, we also started thinking about how this could work within the consultation rooms of healthcare professionals, how this would work together with patients. And there were some studies with so-called decision AIDs. And decision AIDs are sort of booklets nowadays, of course, mostly they're websites, but at that time, they were booklets or even videos for patients. And they were supposed to help patients to think about difficult decisions in healthcare. And research showed that they were very effective in comparison to, say, the traditional ways of communication in consultation rooms.
So if we gave these decision AIDs to patients, they were better informed, they had less regrets, they were less uncertain about the choices they had to make with their healthcare professional. But there were a lot of positive effects at that time. So in the Netherlands, I got a project, I became project leader of a national project to develop these decision AIDs. So we
did this for about five years, and we developed about 20 of those effective decision AIDs. And then we put them on a website. That was about 2010. The next thing, of course we did was we looked at how much these decision AIDs were used by patients, and that was terrible. So the whole implementation of these decision AIDs was a major challenge. And of course, we looked into the literature and studies and they came up with the same results. So we knew at that time that we had a new target or ambition. We should aim at the implementation of shared decision
making. So in 2013/14, I started thinking about ways to improve the implementation in daily healthcare. But it started with those decision AIDs already back in 2006.
Michaella Masters
Brilliant. Because I was just going to go on, and it's a very basic question, I'm sure, as well, why is shared decision making important in medicine? What benefits does it give on both sides?
Haske Van Veenendaal
What do you mean with both sides?
Michaella Masters
Sorry, I mean for the patient and then either for the clinician, the doctor, or the student, etc…
Haske Van Veenendaal
Yeah. Well, for the patient, there are several possible gains.
For example, they have less regret about the decisions that are being made. They're less uncertain, they're better informed. The compliance with therapies is higher, the relationship with clinicians improves.
I always say, just pick the thing that you like, because the results, the effects are major. And this is being shown within a systematic review about every four or five years. And there are over 200 randomized control trials by this time. So, there's a lot of proof that this works. For clinicians, the research that has been carried out is not so extensive, but what we see is that professionals experience that if they perform shared decision making, that the consultations or the discussions they have with the patients are more structured because it has several
models that you can use within your discussion with the patient or the interaction with your patients, they also like that patients are more involved, so they become more active in the conversation that they have together. And also, some clinicians say that it's nice to not have the responsibility of the outcome of the treatments, for example, by him or herself. So it's more a shared responsibility for what happens with the patient.
Michaella Masters
Yeah, of course. So I'm going to ask a couple of questions that are on different levels of expertise so a wide audience can get value out of this conversation. So just kind of going back, how would you explain shared decision making if you had to explain it to a six year old, for example?
Haske Van Veenendaal
To a six year old? Okay, well, I've tried to explain it to my children when they were young.
Michaella Masters
How do you explain it to them?
Haske Van Veenendaal
Yeah, well, the first thing is that there is something to choose. So it's not that one thing is the best to do, but there's a choice to make, and the one choice is not better than the other. All choices are okay. So that's the first thing. And when we are making this choice together, it's important that we know what are the pros and cons of each of the possible choices that we can make. And it's important that we know what you find important as my child or as my patient or whoever you're deciding with. If we put those things together, the perspective of what are exactly the pros and cons, and what is the perspective of the one who is sick or has to make this choice with the clinician, then we always come to a choice that fits with this specific person.
Michaella Masters
And how would you explain it to, for example, a bachelor's student in the medical field?
Haske Van Veenendaal
Well, also that this is a situation in which you have the opportunity to make a choice with your patient. And in this choice, there are several options. They have pros and cons. So you have to explain or discuss the pros and cons of each of the options that are available, and then you have to find out what the patient finds important in relation to the pros and cons of these options so that you can make a well informed decision together, which is also based on the preferences of your patient.
Michaella Masters
Brilliant. And what are the current topics researched or debated amongst the experts at the moment within the field?
Haske Van Veenendaal
There are a lot of topics in research. There has been a lot of work in the past years about models. So models to apply when you're actually in interaction with your patient. So you can say there's a definition of shared decision making, but what does it mean when I'm sitting together with my patient, what do I do? We have developed models, and internationally there's consensus about the model. I think there's always, always debate going on, but more or less we have consensus about what are the most important steps and the content of a good shared decision making conversation. So that's one thing. The other thing is health literacy, of course. So we're able to do this with smart patients that work nicely together with us. But how about the patients that have a lot of trouble understanding information or even to read, like illiterate people. Another research area is implementation. So what I'm doing right now, so we know that shared decision making is effective, but how can we apply it in the right way in each context, for each disease, for each clinician and each patient? Yeah, I think that are some of the topics that are also measurement, so, how do we measure in the right way and what types of outcomes do we need to measure? So that's more the methodology of measurement of SDM.
Michaella Masters
Of course, that actually rolls off very well for my next question, which is, is the structure, or, as you've mentioned, is the models, is it always the same when you're working with a patient? Do you always go through the same set of checklists to make sure that you're having a shared consultation? Shared decision making consultation?
Haske Van Veenendaal
Yeah, I think the steps are very general. Sometimes you need to add things like, if you have a patient that is in chronic care or long term care, then very often you have several diseases within one patient, like comorbidity. And of course, then you have to decide first or discover first what discussion or what type of decision you are going to discuss with the patient. So there's a preparation step, but apart from that, it's very general.
So it's four steps.
First you introduce that there is a decision to make, and what is the role of yourself as the clinician, and what is the role of the patient in the decision making.
And then you have the pros and cons of the options, and you check whether the patient really understands what you have discussed together.
And then the third step is about what is important to the patient, what matters to the patient, what are the patient preferences and values and context.
And the fourth step is bounding this together into a decision that is good for the patient and also supported by the clinician.
Okay, so those four steps are very general. Some models say, well, you have another step, step five, in which you evaluate whether the choices you have made are giving the results that you wanted, and then you start up again with making new choices or adapting the choices you made before.
Michaella Masters
And are there any specific frameworks? I guess this would very much apply to your business with actually training shared decision making. Are there any specific frameworks to learn how to properly do this? Obviously, you've got a set of questions and a set of guides to obviously take depending on the patient. But do you have any frameworks when teaching how to have a shared decision making conversation?
Haske Van Veenendaal
Well, basically this is the framework that I just told you. But when we train, it's all about the specific context in which the clinician works, and that is very different.
So a cancer patient is very different from a child, or a chronic patient is very different from an acute patient, and then you have the role of families, loved ones, you have highly educated people, you have low educated people. So it's very different every time for each clinician. You can work as clinician within a big city, you can work in, how do you call it, local farmers' land, I don't know, pronounce it, say this in English, in a rural area. I guess it's very different each time. And that is why it's so important to train. And what happens often is that clinicians have to integrate the four steps that I just discussed into their own context and situation, and what for them will be the moments that they want to apply these shared decision making techniques. And that is something that takes time and discussion and examples and training, because it's about behavior. Right? So as a clinician, you have to change the way you communicate, and this is about how you think about your role as a clinician towards the patient. Is the patient able to decide about difficult stuff like healthcare decisions? How do I think about autonomy of my patients, about my own role? So, yeah, this is what the training is really about.
Michaella Masters
Okay, brilliant. And what has happened in the last few years in the field? Has there been any significant developments, if you could sum it up?
Haske Van Veenendaal
Well, we're still developing decision AIDs, so it goes on and on and on. And there's always studies about randomized control trials, about decision AIDs for even more and more decision situations. And they keep on showing that the decision AIDs are effective. But what you see now is that there's more research into training, learning, and there's more research into the effects of shared decision making on the organization of healthcare, like finances, guidelines, clinical pathways. So how do we work together as a team?
How does it work within a busy hospital if we want to do this? And, for example, we have to split into the four steps that I just discussed. Sometimes patients need to reflect and have time to think about decisions, but if we have a clinical pathway that doesn't give room for patients to think for a couple of days about the decision to make, then it's difficult to change it as a healthcare team or organization. So it's more research into that. There's more research into low health literacy.
So how can we better inform patients of that? I have trouble taking this information in an easy way.
Michaella Masters
That's perfect. Thank you.
Haske Van Veenendaal
Also very interesting is, for example, in the United States, in England, the Netherlands, Scandinavian countries, shared decision making is pretty popular, so to say. But you see also new countries starting with shared decision making in all different areas of the world. So that's also very interesting.
Michaella Masters
Which regions would you say lead the way with shared decision making training and implementation within medical schools or hospitals, etc?
Haske Van Veenendaal
Yeah, I would say, of course, the United States, because it's a big country. Also Canada. The United States is also always a bit scattered, like, you have one area they're doing a lot, and other areas they don't know, so they don't work on this topic. Canada is very active. The Scandinavian countries, Germany, the Netherlands, I think those are the most. But we also see Taiwan, Australia, New Zealand, Brazil.
Michaella Masters
Yeah, brilliant.
Haske Van Veenendaal
So, of course, Belgium.
Michaella Masters
It's slowly, definitely becoming a bigger force within medical training, it seems.
Haske Van Veenendaal
Yeah. And there's the International Shared Decision Making Society, ISDN, that organizes a congress every two years. So that will be next summer in Switzerland. And if you want to get acquainted with this topic, then this is a very good moment and place to go and find out what is happening in the scientific world of shared decision making, but also in practice. So what's happening with training and implementation.
Michaella Masters
Brilliant.
You mentioned in one of your papers about accelerating implementation of shared decision making in the Netherlands that I believe one of the strategies that you concluded was to increase shared decision making in a way to stimulate the empowerment of patients.
How can you teach your students the balance between, obviously, their professional opinion, but also empowering the patients to choose for themselves?
Haske Van Veenendaal
Well, the patients don't choose for themselves. Share decision making is choosing together. So that's one of the misconceptions that people can have, right? That you put the decision on the shoulders of the patient, but it's really about sharing the decision.
So it's about what role do I have as a clinician and what role can the patient play? And a lot of clinicians would say, well, a patient is not able to decide in the way that I am able to do it because I have had my education, and I'm an expert. I've seen many, many patients. We have our guidelines. We have a lot of knowledge about this disease and the choices to make.
But that's all about the medical side of the choice that you have to make, right? So the thing is that you try to make people aware of that. There's more than only the medical side of making choices and the medical information. There's also the side of preferences and the life of the patient in which this has to come to effect. Right? You make a decision and the patient lives with this decision for the rest of his life or her life. And that's also very important. And if somebody has specific values, if somebody likes to sport, for example, and sometimes you come to different decisions than somebody who likes to play cards with friends in a cafe, right? And that's very important because they will play cards for the rest of their lives if they like to play cards for the rest of their lives, or they like to sport for the rest of their lives, or they like to cook, or they like to take care of their grandchildren or whatever, right? So the choice has to fit in this life. And this is what you don't know as a clinician. The only thing you can do is invite the patient and empower the patient to give this information to you as a clinician to discuss this and to see what choice or what pros and cons fits best with this patient's knowledge or patient situation or patient perspective or whatever you want to call it. I think shared decision making is a very active process of the clinician, but also about getting the patient to be active and tell and share what is important or what matters to him or her.
Michaella Masters
Yeah, definitely. Of course. I know that you did a lot of research as well with cancer patients and oncology care, and I know this very much applies to that because obviously that's on a much harsher scale because obviously it can be terminal. Unfortunately, the diagnosis, and I can imagine that it very much applies to shared decision making, especially within those patients.
Haske Van Veenendaal
Yeah.
Michaella Masters
So. Sorry. Are you okay?
Haske Van Veenendaal
I have to change my light.
Michaella Masters
Okay, that's fine. So I know that you just recently published your PhD. I haven't had the pleasure of reading it yet, so would you mind, I know that it's a PhD, so it's a bit difficult to give a proper summary of it, but would you mind explaining a little bit about what it was about?
Haske Van Veenendaal
Yeah.
The dissertation was about implementation of shared decision making in daily healthcare in clinical oncology care. So, I started with saying that shared decision making is an effective strategy, communication strategy. For me, that's not so interesting anymore to do research at, but I think that it is even more interesting to look at how we can apply this every day in daily care and what is needed to support that or to facilitate or accelerate that. So what we did is we did a study with frontrunners, so people who are already doing this at a higher level, relatively high level, and we gathered them and had interviews with these people about what can we do to accelerate this implementation. And they gave several advices, recommendations about what to do on the national level.
For the Netherlands, that is about empowering the patients, that's about setting good examples in this area. It's about doing implementation work and studies, and to set up effective training strategies, etc. So that was one of the parts of the research. And then we took these recommendations to start up two large implementation studies. In total, eleven teams of hospitals in breast cancer care. And we co-created, with these teams, and together with patient organizations, we co-created an implementation strategy, implementation plan that involves strategy making, tools, training, looking at the organization, looking at the context in which they have to work, like guidelines and finances and stuff like that. What we call a multilevel implementation plan. And we worked with these teams for about a year in two projects. In between, we did an evaluation of the implementation strategy or implementation plan so that we could improve our implementation approach in between.
So we had another three studies, one of six hospitals, then the evaluation, and then another five hospitals. And we showed this multilevel implementation strategy is very effective on the level of application of shared decision making within consultations. So that was our major outcome measure. And the next thing we did was an interview, or, sorry, a questionnaire study among cancer patients, what their experiences are with shadow decision making, and what they need, what they miss in their discussions with their healthcare clinicians. So, for example, they told us that more than 80% of cancer patients also want to discuss the option of no treatment.
Michaella Masters
Okay. Wow.
Haske Van Veenendaal
We're a bit surprised because we knew that patients find this important to discuss also about not treating their disease, but that it would be that high as more than 80%. Yeah, that was quite surprising. And we took this again back to the clinicians, of course, and talked with them about what to do with this finding. And that's very interesting.
We had another study we did about a major barrier for shared decision making. And that is that clinicians think that shared decision making takes more time. So if you do more shared decision making, people are afraid that it will take more time. So we did a systematic review and meta analysis and we showed that it looks like that it doesn't have to take more time. So there were 35 studies that we selected and 28 of those studies do not show an increased level of consultation duration.
Michaella Masters
Okay.
Haske Van Veenendaal
The only question that remains is whether there's a temporary increase of consultation time so that after, for example, you do a training or you use decision aids within your consultation or in your clinical pathway, that it temporarily increases the consultation duration. And after a while, when you're used to working with these new habits or the new decision tools, that it doesn't take more time anymore. But we don't know that. There's two literatures done on that question.
And the last part of my dissertation is about a study protocol in which we study the effect of individual feedback and coaching on audio recorded consultations. So we find out in the other projects that we did that feedback on giving feedback on recorded consultations is effective, but we want to see whether we can scale it up on a national level. So we included 14 hospitals in our study and we digitized the whole approach so that we think we could scale it up more easily. But that's only protocol. So this study is not finished yet.
Michaella Masters
Okay, brilliant. Well, I was actually just going to ask you, we know you because you use Videolab. Would you be able to tell us a bit more about how you've used it, what training did you use it for and why did you pick Videolab to start with?
Haske Van Veenendaal
Yeah, we were looking for a system to safely record consultations. When I started with my PhD, there was a good instrument to look at consultations, to observe what happens within the consultation room as it comes to the level of shared decision making that clinicians apply. But the thing was, it was only used for research purposes. So a lot of consultations were recorded by video or audio or observed by an observer within the room, and they were also scored. You can give a score on a level of zero to 100, and zero is no share decision making. 100 is the best shared decision making you can accomplish. But it was only used for research purposes. And what we did is when we talked to patients and clinicians, they said, we want to know what comes out of this observation, so we want to have this feedback to see whether we can improve. So we started to develop feedback forms for clinicians. And then we also needed, of course, a simple system to safely record these consultations. And we're working with eleven hospitals beginning of our projects, and this study we're doing now, another 14 hospitals so it needs to be safe, it needs to work at every place, and we need to be able to approach it from the place where I work, like within this room or wherever I am working. So then we looked at different systems that would support this recording. And via our network, we got in contact with CODIFIC and Videolab. So we tried it and we were very positive about it.
Michaella Masters
Brilliant.
Haske Van Veenendaal
So we started using it.
Michaella Masters
I'm very glad you find value in it. That's the whole point of the system, is to be as valuable as possible for exactly your use case. Where do you think Videolab could be used in the future, if you've ever reflected on it after now having experience with the system, knowing how it works very well?
Haske Van Veenendaal
Well, for shared decision making. In the Netherlands, we are trying to see this giving feedback on consultations as a very normal, regular training approach for clinicians. So I believe that you need to train your communication techniques, like regularly, say every two years, you need to do a training or record a series of consultations and get feedback and coaching from an expert.
So I think for scaling up this whole idea of training your communication competencies, it's very important to have such a system that facilitates this. Yeah. And I think that what would help is that we're also starting to think about how we can also provide the patients to listen to this consultation that has been recorded, for example, and maybe every consultation, and then have it in the, how do you call it, the electronic record of patients.
Michaella Masters
They're able to go back.
Haske Van Veenendaal
And they can listen back with their family, for example, and if they have questions, discussion within the family, and then again go back to the hospital for questions.
Michaella Masters
Okay, wow, that's very interesting.
So I actually only have one last question, which is a little bit of a kind of concluding question, and it's how do you see the future of healthcare? And what are some of the most important things that you would have changed in the next decade?
Haske Van Veenendaal
Yeah, for me, of course, it's about sharing decisions, but I think shared decision making is a way, a strategy to change health care in the right direction.
I think two things are very important in the healthcare of the future. One is equality. And that means that within healthcare, as a clinician and patients, we are all humans, right? So we are equal. As human beings, we all have our own qualities and expertise, and we need both expertises to come together to make the right decisions for the lives, the daily lives of the patients that we help as clinicians. So we need to really feel that equality is prerequisite. So something that should be the standard for us. So that's one thing. And the other thing is, of course, we are equal, but we are all different. So in order to do this in the right way, we need to acknowledge that every patient and every situation is different. And also clinicians are different because they're also human beings. So the art or the challenge is to have the power to do the right thing in each situation. And that is what we call equity. So in each specific situation, you need to do something different. And I think this is about learning how to do this and keep on learning in very difficult situations, very difficult decisions sometimes that clinicians make with their patients. It's the most important thing to train and to keep on learning.
Michaella Masters
Yes, definitely. Well, thank you so much. First of all, those are all the questions that I have. Of course, you can have the floor. If there's anything that you would like to bring up that we haven't spoken about, please feel free to. I know that I've asked you loads of questions.
Haske Van Veenendaal
Thank you for the questions and the discussions we had together. And if there are any questions of other people coming towards you or they can also approach me, of course, I'll be happy to answer.
Michaella Masters
Well, thank you so much. And I look forward to actually reading your PhD. I definitely think it sounds extremely interesting, especially when you have used Videolab, you know, the use cases, and in general, just with shared decision making, implementation methods, etc. So, yeah, thank you so much for your time and have a lovely evening.
Haske Van Veenendaal
Thank you so much.
Michaella Masters
Perfect. Thank you very much Haske.
Haske Van Veenendaal
See you later.
Michaella Masters
Thank you. See you later. Bye.
