Updated: 5 November, 2024
Introduction to Feedback in Healthcare Training
Key takeaways:
- The importance of feedback in healthcare should not go unnoticed. Feedback helps doctors identify their strengths, areas for improvement, and work towards enhancing their effectiveness.
- Correctly delivered feedback gives people the ability to manage, develop and improve performance much more efficiently.
- There are very typical feedback methods such as summative and formative, and there are less common feedback methods such as video-based feedback, The Pendleton Model.
- Patients and doctors are capable of leaving healthcare providers due to poor communication.
- The results of a study (more below), proved that 90% of students noticed an improvement in their communication skills through video based observation and evaluation.
Purpose of feedback
The importance of feedback in healthcare is paramount, it is an integral part of all education, training, and daily professional activities in most European countries. It serves as a valuable tool for assessing progress and determining whether a redirection is needed. In the healthcare field, feedback is especially important for providing doctors with insights into their practice from the perspectives of their colleagues (2).
Through feedback, doctors can identify their strengths, areas for improvement, and work towards enhancing their effectiveness. Junior and senior doctors may request feedback or their peers may approach them for feedback. However, all parties involved may find giving and receiving feedback is not without its challenges.
Who does it benefit?
The ability to give and receive feedback is crucial for successful performance management and development. It is essential in directing individuals’ focus and energy toward accomplishing objectives in the most efficient manner possible by promoting clarity and alignment. Feedback can be either constructive, by identifying mistakes or opportunities for improvement, or appreciative, by acknowledging accomplishments or recognising the value of someone’s contribution. Engaging in transparent feedback and collaborating with others allows for performance improvement. Other benefits of feedback include (5):
- Feedback helps them improve their skills and knowledge, and make necessary adjustments to improve patient care.
- It prevents performance from going off track and wasting valuable time, energy and resources.
- Giving appreciative feedback and recognition builds confidence and a sense of being valued.
- When delivered effectively, feedback can improve the quality of working relationships within a team.
- For patients, feedback provides a way to express their concerns, experiences and opinions about the care they received. This helps healthcare providers to provide more patients-centred care.

Feedback consequences
Feedback comes in a variety of forms and directions. The most typical one being tutor to student feedback, then there is peer to peer feedback, tutor to tutor feedback and so on. Lastly, a less common, however very powerful feedback, patient to student/ doctor feedback.
According to a Patient Perspective study, 36% of patients have left a healthcare provider due to poor in-person experience and lack of communication.
In every business, we ask our customers for their feedback, however tough it may be, we want, and need, to learn what our customers think about our product and most of all, how they feel about it. Therefore why is it less common to ask patients for their feedback on their healthcare experience? The importance of feedback in healthcare is stronger now than ever, and this will only increase. Patient feedback helps doctors have a clear picture of patient expectations and how to improve care (6).
Difficulties of delivering and receiving feedback in medicine
Certain barriers in the feedback process can limit the depth of feedback that an individual receives. As a result, this can have consequences on the level of education they receive, as well as their opportunities for improvement and success. Some of these barriers include:
- Avoid making feedback too personal and hurting feelings:
- Feedback can be difficult to deliver if the assessor believes the feedback may disappoint or upset the learner.
- However, the desire to avoid upsetting the learner can lead to a phenomenon known as “vanishing feedback”, where meaningful feedback is avoided.
- Lack of knowledge:
- Giving and receiving feedback requires an understanding of both the process and the skill. If either the assessor or the learner lack these, the learning outcomes will not be as beneficial nor effective.
- Lack of external feedback:
- When external feedback is not available, students may resort to self-assessment, but this approach is often prone to error. Research indicated that high performers tend to underrate their performance, while lower performers tend to overestimate their abilities.
- Lack of direct observation:
- The effectiveness of feedback is highest when it is based on the direct observation of the task. In a busy clinical setting, direct observation is often not feasible, which can limit the impact of feedback due to the lack of opportunity for such observations. (3)
Essentially, all the above points can be managed correctly to allow the best out of a student’s education. Ultimately the importance of feedback in healthcare and, in any other sector, is that it allows the learner to better their abilities, knowledge and skills of said task. Learning is a continuously cyclical process.
Different feedback methods
There are many types of feedback in medical education. They can vary very much with styles and types. The typical ones such as Formative and Summative feedback. Formative feedback being a student’s progress throughout a course, where they are given consistent feedback, reflection and redirection feedback throughout the progress of learning a new skill. Summative feedback measures performance, commonly against a standard yet by the national health organisation in each country. Summative feedback is typically given with a grade or mark that ranks individuals or groups. (2)
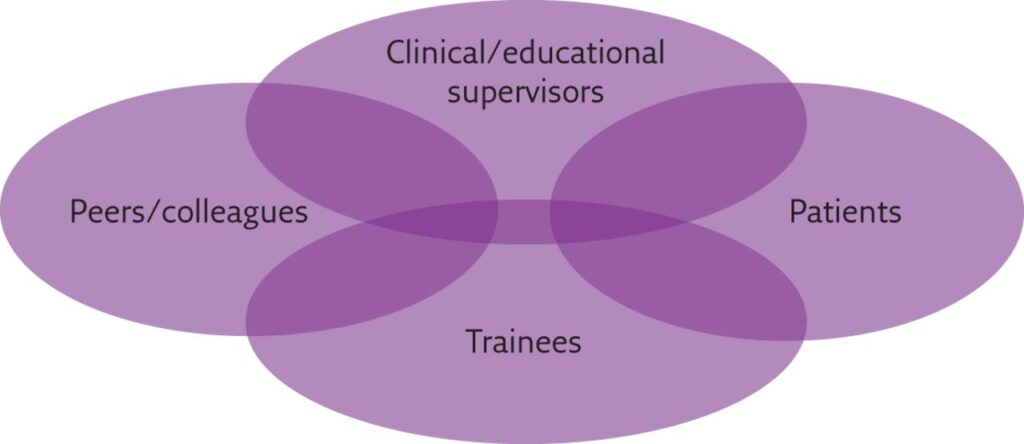
Below shows a figure which demonstrates the different feedback sources in healthcare. Retrieved from (2)
There are other feedback methods such as:
- The feedback sandwich:
- The feedback sandwich involves starting and ending with positive feedback, with critical feedback sandwiched in between. This can be useful in clinical practice, but overuse can reduce its effectiveness as the receiver will anticipate negative feedback. It is important to also give positive feedback separately when possible, to help colleagues feel valued and open to feedback
- Chronological fashion feedback:
- This is pretty self-explanatory. When reflecting on the observations from the start to finish of a learning session, the person giving feedback provides it in chronological order.
- The Pendleton Model:
- Developed in 1984, the Pendleton model is a learner-centred and conversation-based feedback model. It focused on creating a safe environment for feedback by first highlighting positives before identifying areas for improvement. The model uses open questions to encourage reflection.
- E.g. “What do you think went well?” , “What do you think could be done differently?”, “How can this be achieved?”.
In healthcare and overall education, people use many other feedback methods besides these few examples.
Research done on Feedback models/ methods
Research published in the Health Professions Education, Sep. 2018, described a study done on the perception that students have when given feedback. Diving deep into which feedback method they find most useful and effective.
Results came back showing students preferred receiving feedback in a private dialogue which contains a mixture of positive comments, followed by areas of improvement. It also found that comparing students’ performance against each other made the feedback disregarded and unspecified, therefore, unhelpful for students. Furthermore, students recommended applying peer feedback and mutual feedback regularly in a safe and open environment.
The conclusion of the study outlines that students require continuous constructive feedback, mutual and peer feedback, and a balance between positive and points for improvement.
It is important to note that students were also heavily influenced by the way feedback was delivered by a faculty member. If there was lack of time or poor communication skills from an accessor, students found this feedback difficult to process. (1)
Our experience…
At Codific, our Growth Strategists have interviewed over 250 healthcare professionals involved in the assessment process of students in both clinical and communication environments. We have gathered a lot of information about the feedback styles in the different countries and different faculties. Within the UK, many traditional feedback methods are still used. Many universities give direct feedback directly after a consultation or examination. The teacher usually delivers it to the student, offers them some time for reflection, and gives feedback through written assessment. Alternatively, a newer feedback method is becoming much more popular in Northern Europe through video recording. This structured feedback approach assesses students through reflection on their video consultation with either simulated patients or real life patients. Giving students the opportunity to watch back how they did and what they felt they could improve on.
Due to this, in the following we will be going deeper into these two feedback methods used in healthcare teaching, direct feedback and video-based feedback and reflection.
Comparison of video-based feedback and direct feedback
A study done by researchers in the University of Geneva, Faculty of Medicine (4) explored the comparison between direct feedback, where students observed practising clinical skills with simulated patients and given verbal direct feedback after the encounter directly afterward. Or, the latter, where both students and supervisor would review the videotaped encounter and deliver feedback.
Students felt more engaged during the video-based sessions as they felt it facilitates a more active role and room for discussion of clinical reasoning. They also made the observation that video feedback was more useful for improving some clinical skills.
Researchers from the National University of Singapore published another study (7) on nursing students’ experience receiving peer video feedback. The study found that some students found video feedback more stressful than direct feedback. However, it was very useful for them as it provided evidence of their performance, allowing for deeper reflection. The study concluded on how many faculty members believe that both video based feedback and direct feedback should be part of the nursing curriculum.
More studies…
Another study achieved similar results, based on “Video training with peer feedback in real-time consultation” (8) by professors at the University of Leuven. It involved trainees of the general practitioner master program, who received video training with peer feedback in real-time consultation. Approximately 70% of trainees had a positive view of recording consultation, however 60% of them believed that their patients felt uncomfortable during the recorded encounter. With that in mind, close to 90% noted an improvement in their communication skills through video based observation and evaluation. Overall, the study emphasizes the potential of video training in real-time consultations and suggests that communication skill training underestimates the power of visual learning.
Other studies on video based feedback, such as (9) published in the BMC Med Educ, found that the main benefits students received from video-based feedback were; the deeper analysis on self-perceptions, reflective practices, peer-feedback and heightened focus on patient-centred approach to healthcare. Quantitative study (10) done around the effectiveness of video-assisted debriefing (VAD) in simulation-based health, established that “VAD improved learning outcomes and offered comparable benefits as verbal debriefing.”
The importance of feedback in healthcare is incomparable, just these few studies show the tools available to facilitate the medical education process.
Author’s opinion
There is an obvious advantage of using video based feedback from the results and feedback of the studies. However, a small matter appears to be present regarding the level of comfort experienced by students and patients during recording. The decision here depends on two things. Firstly and foremost, recording patient consultations requires consent, which should be obtained either verbally or preferably in writing. Some universities ask for double consent, once before the consultation and again after the consultation. This gives patients the opportunity to feel their most comfortable throughout the session. If there is doubt in their mind after the consultation, they are able to retract the consent.
Secondly, when evaluating the benefits the students receive by using video-based feedback compared to the slightly uncomfortableness they can feel throughout. One must weigh these to evaluate which better compensates results and performance.
Additional comment: students typically feel uncomfortable the first time they are recorded, which is a normal reaction. Video-based feedback is a newer tool that has been introduced in recent years, and not everyone has had the experience yet.
How does Videolab contribute to video feedback?
Videolab is a privacy compliant video sharing platform where students and professors can record a consultation in a GDPR safe environment. Students can upload a simulated consultation, peer-to-peer consultations, or real patient consultations, and the platform encrypts them at the source. Videolab then allows for self reflection by tagging and annotating time fragments for both the student and the teacher.
Users can provide feedback and evaluations on specific time fragments or the whole video, using structured evaluation methods according to defined evaluation methods. All the measures are out in place for patient interactions training to be easy, efficient and secure.
Videolab includes many different feedback directions (see image below).
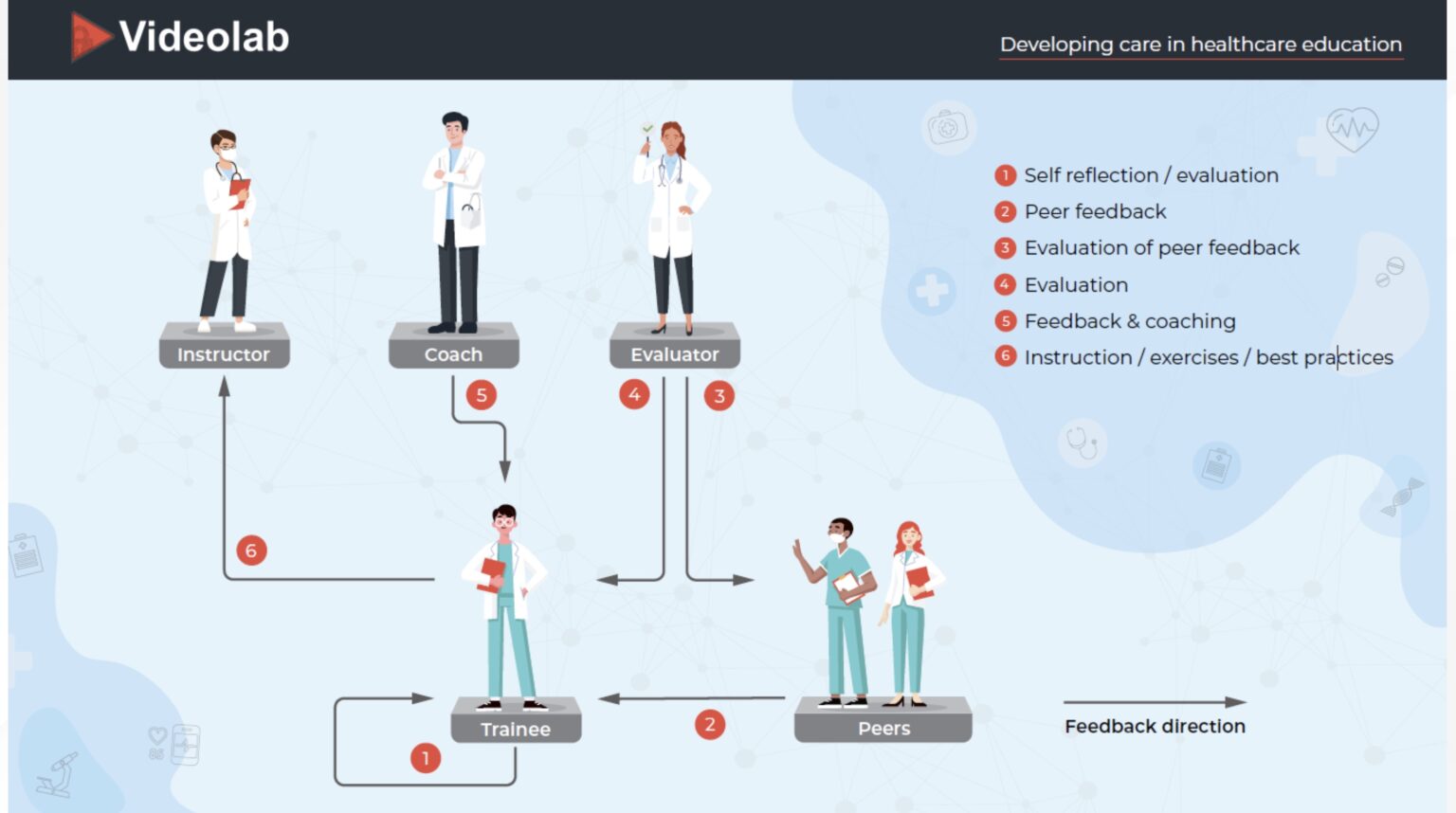
According to the conclusion in study 7, how nursing found a combination of video-based and direct feedback would be the most beneficial toward learning. With Videolab, this is possible as it can be used for both purposes!
If a consultation is in session, and is being recorded, feedback can be given directly after the session, and uploaded onto Videolab afterward. This gives the students an opportunity to watch and reflect on their performance and add any further comments. And lastly, share with additional pre-approved assessors or peer for additional feedback.
Conclusion
In conclusion, feedback is an essential tool in healthcare that helps doctors identify their strengths, areas for improvement, and work towards enhancing their effectiveness. It benefits patients by providing a way for them to express their concerns, experiences and opinions about the care they received, helping healthcare providers to provide more patient-centred care.
Ultimately, the choice of feedback method depends on the learning goals, the context, and the preferences of the instructor and student. Using a combination of feedback methods can be beneficial in providing a more well-rounded learning experience.
References
- Alfehaid, S.L., et.al. (2018). The Perceptions and Attitudes of Undergraduate Healthcare Sciences Students of Feedback: A Qualitative Study. Health Professions Education. Volume 4 (3). Pp. 186- 197. https://doi.org/10.1016/j.hpe.2018.03.002
- Hardavella, G., et. al. (2017). How to give and receive feedback effectively. National Library of Medicine. 10.1183/20734735.009917
- Burgess, A., van Diggele, C., Roberts, C. et al. (2020). Feedback in the clinical setting. BMC Med Educ 20 (Suppl 2), 460. https://doi.org/10.1186/s12909-020-02280-5
- Perron, N., Louis-Simonet, M. Cerutti, B. et, al. (2016). Feedback in formative OSCEs: comparison between direct observation and video-based formats. Medical Education Online. Volume 21 (1).
- Giving and Receiving Feedback. Quick Reference Guide for Managers. (2014). https://www.publicsector.sa.gov.au/__data/assets/pdf_file/0005/219821/009-Giving-Receiving-Feedback-Managers.pdf
- PatientPop. (2022). 4 ways patient feedback can help improve your healthcare practice. https://www.patientpop.com/blog/4-ways-patient-feedback-improve-healthcare-practice/
- Yoong, Si. Qi., Wang, W., Kim, S., et,al. (2023). Perceptions and learning experiences of nursing students receiving peer video and peer verbal feedback: a qualitative study. Assessment & Evaluation in Higher Education. https://doi.org/10.1080/02602938.2023.2184462
- Eeckhout, T., Gerits, M., Bouquillon, D. et, al. (2016). Video training with peer feedback in real-time consultation: acceptability and feasibility in a general-practice setting. National Library of Medicine. 10.1136/postgradmedj-2015-133633
- Dohms, M.C., Collares, C.F. & Tibério, I.C. (2020). Video-based feedback using real consultations for a formative assessment in communication skills. BMC Med Educ 20, 57. https://doi.org/10.1186/s12909-020-1955-6
- Zhang, H., Morelious, e., Goh, S. et, al. (2018). Effectiveness of video-assisted debriefing in simulation based health professions education: A systematic review of quantitative evidence. 10.1097/NNE.0000000000000562
