Updated: 8 December, 2025
Mirroring body language is a communication behavior where one person subtly copies another’s nonverbal cues during an interaction. When used effectively, it can help medical students and clinicians build rapport faster and help patients feel heard and understood, which is key for patient-centered care and shared decision-making.
This technique is already part of soft skills training in many clinical education programs. Its value becomes even clearer when interactions are reviewed with video, giving learners direct insight into how small gestures affect patient responses. While it may seem like a subtle detail, mirroring shapes how providers are perceived and how relationships develop.
What Is Mirroring in Body Language?
Mirroring in body language involves subtly reflecting another person’s gestures, posture, facial expressions, or tone of voice. Often unconscious, this behavior contributes to a sense of connection and trust. Psychologists describe it as part of the chameleon effect – an automatic adaptation that supports social harmony (Chartrand & Bargh, 1999).
In healthcare education, mirroring is being taught more intentionally. For instance, doctors who learn to match a patient’s posture or tone often find it easier to navigate sensitive conversations. This practice draws on findings from neuroscience, particularly around mirror neurons. These are brain cells that activate both when we act and when we observe someone else doing the same (Gallese & Goldman, 1998). This shared activation helps us understand and empathize with others, making mirroring a powerful mechanism for social learning and emotional connection (Rizzolatti & Sinigaglia, 2010).
Why Mirroring Matters in Healthcare Training
Mirroring supports empathy, active listening, and presence. Used skillfully, it helps patients feel seen and encourages them to speak more openly. In training, it develops awareness of nonverbal communication and helps students practice adapting to diverse clinical situations, including breaking bad news or negotiating treatment decisions.
In team settings, mirroring also supports smoother collaboration. When body language aligns, it reinforces shared goals, particularly under pressure. Simulation and video review help learners recognize these patterns, showing how posture and tone can build trust or unintentionally create distance.
The Psychology and Neuroscience Behind Mirroring
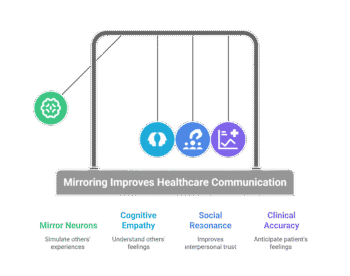
Mirroring body language is supported by well-established research in psychology and neuroscience. The neural activity of these mirror neurons supports what’s known as cognitive empathy – the ability to understand another person’s feelings and intentions without necessarily feeling them yourself.
At the center of this behavior are the mirror neurons we mentined before, whose dual activation allows us to internally simulate another person’s experience, laying the groundwork for empathy, rapport, and what’s known as “social resonance” (Gallese & Goldman, 1998). This is closely tied to the theory of mind, which refers to our ability to infer the mental states of others. Together, these processes allow healthcare providers to anticipate how patients might think or feel, improving both connection and clinical accuracy.
Experiments by Chartrand & Bargh (1999), revealed that people who were subtly mirrored felt more at ease and connected to their conversation partners. Subsequent research confirmed that this kind of mimicry increases interpersonal trust, improves likability, and even enhances cooperation among strangers (Lakin et al., 2003).
Research by Reilly et al. (2012) shows that drama-based medical education increases students’ awareness of body language and improves empathic communication through role-play exercises. This hands-on approach helps learners internalize nonverbal cues rather than memorize them.
In digital environments, mirroring still matters. A 2023 study by Mazouri et al. found that patients preferred video consultations where clinicians used expressive facial cues, direct eye contact, and full upper-body framing. These findings reinforce the importance of visual empathy, even through a screen.
Practical Examples in Clinical Training
Mirroring body language can be practiced effectively in clinical training through simple but focused activities. One of the most useful is simulated doctor-patient interaction. These sessions create space to try out subtle gestures, adjust tone, or match posture in real time, giving students firsthand experience with trying out what works best for them.
Another method is interprofessional feedback. During group simulations, students can work with peers across disciplines (nursing, psychology, or pharmacy) to see how nonverbal behavior shifts in team dynamics. They often get real-time feedback on how their body language affects collaboration, especially when mirroring helps reduce tension or clarify intent. This kind of exercise promotes reflection and improves communication across the board.
Video analysis is where everything comes together. With a tool like VideoLab, students and educators can record clinical role-play sessions and review them to spot patterns they may have missed in the moment. For example, they can see if they leaned in when the patient did, or if they unintentionally mirrored a defensive posture. These moments become teachable, and learners start recognizing what mirroring looks like when it works and when it doesn’t.
Videolab makes it easy to annotate and share clips securely, offering peer and instructor feedback all in one place. This kind of guided reflection supports more than communication, it strengthens awareness, builds soft skills, and enhances empathy.
Benefits and Risks of Mirroring
Thoughtful mirroring improves communication by reinforcing empathy and trust. When a healthcare provider mirrors a patient’s posture or tone, it often makes the interaction feel more personal. This can encourage openness, especially during conversations involving fear, confusion, or hesitation.
Another benefit is enhanced communication. Mirroring often supports active listening without interrupting the flow of conversation. It also creates a nonverbal bridge between doctor and patient that reinforces verbal messages. This can also signal respect and reduce perceived social distance.
However, mirroring is not without risks. If overused or done too obviously, it can seem forced or even manipulative. Patients may notice when mirroring feels rehearsed or inauthentic, which can damage rapport instead of building it. For instance, copying a patient’s gestures too closely or too quickly may come off as mimicry rather than empathy.
That’s why authenticity is essential. The goal isn’t to perform a script, but to stay present and responsive. Practice and reflection help make mirroring feel natural.
How to Teach Mirroring Skills in Medical Education
Teaching mirroring skills in medical education works best when students can see and feel the effects of their own nonverbal behavior. One proven method is role-play. During structured scenarios, students interact with simulated patients and focus on matching tone, posture, or facial expressions in a way that feels natural. Instructors can guide these sessions by pausing to explore when mirroring helps build connection and when it might feel off.
Adding simulation further enhances this. In controlled settings, students face emotionally charged situations (like calming an anxious patient) where subtle mirroring can shift the dynamic. These moments help learners experience how body language can support empathy and trust, even before a single word is spoken.
However, most of the learning happens afterward. Through video-based self-reflection, students watch their own recorded interactions and begin to spot unconscious cues. Peer review also plays a role. Watching and commenting on each other’s recordings teaches observation skills and highlights what effective mirroring looks like in practice. According to research on reflective training (Noordman et al., 2019), combining self-review with structured feedback improves communication outcomes and empathy scores.
Conclusion
Mirroring body language isn’t just a communication trick, it’s a valuable tool that supports empathy, builds rapport, and enhances patient-centered care. In medical education, learning to mirror effectively can help students become more observant, more reflective, and more attuned to nonverbal cues that often go unnoticed.
Structured training makes this possible. Through role-play, feedback, and video analysis, learners begin to understand the impact of subtle gestures and expressions. These insights not only improve individual performance but also strengthen team communication and interprofessional collaboration.