Updated: 14 May, 2025
The doctor-patient consultation is a key component of healthcare delivery. The relationship between a doctor and a patient is an important relationship in which information is shared, diagnoses are made, and treatment plans are developed. While the specifics of each consultation differ depending on the patient’s needs and the doctor’s skill, most consultations follow a common format. Understanding this structure can enable patients to participate more effectively in their care. This enables healthcare professionals to provide more effective treatment. In this article, we’ll look at the common steps of a doctor-patient consultation and how healthcare professionals are able to obtain this skill.
Key Takeaways
- Structured consultations improve both patient experience and clinical outcomes
- Structure saves time and improves efficiency
- The Calgary-Cambridge Guide provides a framework for structured consultations
- Doctor- patient consultations can be trained

4 Factors why structure is important in a doctor-patient consultation
According to EUSTATS in 2021, the frequency of medical consultations differed significantly among EU nations. The average number of yearly doctor consultations per inhabitant ranged between 3.5 and 7.8 in most EU member countries. Considering the amount of people living within the EU it is needless to say that the quality of those consultations highly impacts the general healthcare environment in a country. Concrete 4 factors highlight the impact on both patient and doctor.
Patient Experience
Structured evaluations help doctors to ensure that the patients feel heard, understood, and participate in their care by setting clear expectations, steering the conversation to important topics, and actively listening to their concerns. This strategy increases patient happiness, improves therapeutic results, and lowers anxiety by giving your patients a sense of control and predictability.
Clinical Outcomes
A structured consultation improves the clinical outcome. Doctors can use a standardised approach to understand the patient’s symptoms and medical history. This helps in lowering the possibility of overlooking crucial information and improving diagnosis accuracy. Through data collection, doctors are able to create personalised treatment programs for each of their patients. This takes into account individual patient’s needs, including aspects such as medical history, lifestyle, preferences, and other potential dangers. Structured consultations can strengthen patient-doctor interactions by encouraging open and honest communication, resulting in a better understanding by patients of their condition and treatment plan and, ultimately, better clinical outcomes.
Efficiency and Time Management
With the number of people visiting a doctor every year, time and efficiency is crucial to ensure a well-functioning healthcare system. This can be achieved through structured consultations, which set up a framework for time efficient and effective doctor-patient interactions. Structured consultations improve the use of the limited time available by directing the talk to key subjects and prioritising information collecting. This targeted approach enables clinicians to quickly and precisely assess the patient’s health, identify potential diagnoses, and discuss treatment choices, thereby saving a lot of time. Structured consultations may also simplify administrative activities like note-taking and record-keeping, reducing the stress on healthcare personnel and increasing efficiency.
Legal and Ethical Considerations
Healthcare professionals regularly find themself in legal disputes with their patients. A structured consultation sets up a thorough framework for guaranteeing legal and ethical compliance in healthcare interactions. Using standardised forms or templates allows doctors to keep clear and consistent documentation, lowering the possibility of misunderstandings or mistakes that could lead to legal challenges. Structured consultations also serve to guarantee compliance with important legal and ethical norms, such as informed consent, patient confidentiality, and professional conduct, which protects both patients and healthcare practitioners from legal ramifications. Furthermore, well-documented structured consultations can serve as proof of adequate care, lowering the possibility of malpractice claims and establishing compliance with professional norms. This not only protects the individual healthcare professionals who have to do multiple consultations per day but also reduces the burden on the legal system of the country. (Source)
Calgary-Cambridge guide to medical interviews
So how is a doctor-patient consultation structured? The Calgary-Cambridge guide to the medical interviews is a widely recognised model for assessing communication skills between healthcare professionals and their patients. Initially developed by Kurtz and Silverman at the University of Calgary and the University of Cambridge, this guide offers an organised way to conduct medical interviews, with the aim of improving the quality of patient care and the effectiveness of clinical interactions. (Source)
Goals of the Guide
Its fundamental objectives are divided into two main areas. First of all, building an effective relationship and providing a clear structure for interviews between doctor-patient consultations.
- Building an effective relationship should be one of the main goals for a doctor during a consultation because it facilitates and encourages open communication. The patient, feeling more valued and understood, is more willing to share vital information which benefits a more accurate assessment. Additionally, an effective relationship promotes empathy and understanding. Also, a warm and respectful communication environment can reduce the patient’s stress and anxiety. Thus allowing them to feel as though they are in a trustworthy environment.
- The second goal is to provide a clear structure for interviews. The guide offers a detailed outline that covers all stages of the interview, from opening to closing. This systematic organisation helps doctors maintain a coherent approach and ensure that all necessary aspects are addressed during the consultation. This allows doctors to better manage time while ensuring that all relevant information for diagnosis and treatment is obtained. Ultimately, it contributes to a more organised and professional experience for the patient, which can lead to greater effectiveness in medical care.
The Calgary-Cambridge model divides a doctor-patient consultation into five phases. Each phase has specific objectives and skills that healthcare professionals develop and apply during doctor-patient consultation. These phases guide practitioners through a structured approach to patient interaction, ensuring comprehensive and effective communication throughout the medical interview. (Source)
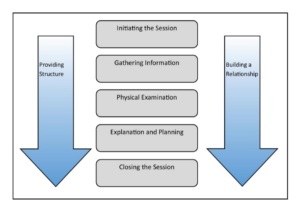
Structure of the Model
Phase 1: Initiating the Session
This phase focuses on preparation and establishing a relationship with the patient. It begins with creating a comfortable environment, introducing oneself, and explaining the purpose of the consultation. It is essential for the healthcare professional to show empathy and respect for the patient’s concerns from the start. (Source)
Phase 2: Gathering Information
In this phase, the goal is to obtain a complete and accurate medical history. Using different types of questions, both open-ended and closed, the symptoms, past medical history, and family and social backgrounds are explored. It is crucial to listen actively and show genuine interest in the information provided by the patient. (Source)
Phase 3: Examination
During this phase, a physical examination is conducted based on the information previously provided. It is important to explain each procedure to the patient. Further, the healthcare professional needs to obtain consent, ensuring their comfort and safety during the examination. (Source)
Phase 4: Explanation and Planning
After collecting and analysing all the information, the healthcare professional must explain the findings to the patient in a clear and understandable manner. Possible diagnoses and treatment options are discussed, and a joint decision is made on the action plan. The patient’s active and conscious participation in this phase is essential for their adherence to the treatment. (Source)
Phase 5: Closing the Session
The interview concludes with a summary of what was discussed and a clear follow-up plan. The professional must ensure that the patient understands all the information and that all their doubts are resolved. The availability for future consultations is reinforced, and contact information is provided if necessary. (Source)
How self-reflection can be beneficial to doctor-patient consultations
The key to mastering a doctor-patient consultation besides having a proper structure in place is both verbal- and nonverbal communication skills. For some people this aspect feels very easy and natural but others who struggle to communicate effectively have to train this. This is where self-reflection comes in, enabling trainees to connect previous experiences to current problems.
This improved understanding allows them to make better decisions in the future. Reflection helps medical trainees recognise their own strengths, shortcomings, prejudices, and emotional triggers. This self-awareness enables people to find areas for personal and professional growth.
Furthermore, reflecting on patient encounters helps trainees grasp the patient’s point of view and feelings. This builds empathy and compassion, which are essential skills for developing trust with your patients and their families.
How Can Videolab improve your doctor-patient consultation
Videolab is a safe video recording tool that enables trainees to connect past experiences to current problems. This helps the trainees to learn a proper doctor-patient structure by receiving feedback through multiple sources such as peer feedback, self-reflection, direct coaching, or a structured evaluation.
These multiple feedback sources help medical trainees recognise their own strengths, shortcomings, prejudices, and emotional triggers. Self-awareness enables people to find areas for personal and professional growth.
How Videolab works:
Trainers or trainees are able to safely record a patient consultation either through their skills labs camera set up with CloudControl or with the Videolab Recorder application. This recording is encrypted upon upload and is not stored anywhere else. Trainers or trainees can review and reflect on the recording, adding time-fragmented feedback where they feel necessary. Then they can safely share this recording with peers, or different experts and instructors across their organisation. Additional structured evaluation can be added and feedback can be connected to whatever learning management system is in place.