Updated: 19 November, 2024
Teaching with patients is a crucial part of medical education, research has shown that recording patients and using videos facilitates discussions of clinical reasoning, communication and professionalism while actively engaging students as mentioned in Perron et al. (2016). This article focuses on the topic of video recording patients. In it we go over the benefits of it and the ethical considerations and privacy concerns that should to consider.
Key takeaways:
- Recording patients for educational purposes can have positive effects on training communication skills and learning outcomes, as evidenced by various studies. It can be a practical tool for teaching, allowing for self-reflection and peer-to-peer feedback.
- Patient comfort and consent are crucial considerations when deciding to record patients.
- Video recording patients is legal and ethical when proper consent is obtained according to GDPR guidelines. Consent must be freely given, specific, informed, and documented.
- To ensure best practice, we recommend using an application that encrypts the video immediately as it is recorded, such as Videolab.
Why should you record patients?
Recording patients comes with several benefits to medical education. Dohms et al. (2020) presents evidence that providing video-based feedback using real consultations appears to be associated with significant increases in self-perceived empathy. Moreover, the use of video feedback was linked to a deeper level of self-assessment, peer-feedback, and reflective practices.
In addition, Eeckhout et al. (2016) indicated that 70% of the GP trainees were positive about recording consultations and almost 90% noticed an improvement of their own communication skills. As well, both students and teachers in the field of medicine were found to acknowledge the underestimation of the power of imaging in the training of communicational and vocational skills.
Finally, Zhang et al. (2022) postulates the benefits of video-assisted debriefing by evidencing that it improved learners’ experience, attitude, and performance. This type of debriefing improved learning outcomes and offered comparable benefits as verbal debriefing.
The studies mentioned above show that recording patients and using videos in training does help in improving both nonverbal communication skills and verbal communication skills. Communicational skills are crucial for providing quality healthcare and patient safety. Being a good communicator can allow a doctor to more easily obtain required information from patients. At the same time this ensures the patient’s comfort and understanding which increases the probability of correctly following treatments. If you want to learn more about the importance of communication skills in healthcare then I recommend you go to this article, for now, let us go back to the topic of video recording patients.
When should you not record?
Although video recording patients has its proven benefits for medical education it might have detrimental effects for patients if not done carefully. Eeckhout et al. (2016) shows that GP trainees believed that in 60% of cases patients felt uncomfortable during video-recorded encounters. Thus, it is crucial to record patients carefully and with consent, to ensure their comfort.
Although recording patients for medical education may have benefits, it is vital to prioritize patient care above all. Patients need to feel comfortable with their doctors. Therefore, one should only record patients when they feel fully comfortable with it and understand the purpose of the recordings. This leads us to consider the legal and ethical considerations when video recording patients.
Is video recording medical patients legal and ethical?
In general, recording medical patients is legal if the patient has consented to it. In the European Union the rules around the use of data are stipulated in the General Data Protection Regulation (GDPR).
But what entails consent from a patient. According to the GDPR, obtaining consent from a data subject is subject to several rules, including:
- Consent must be “freely given, specific, informed and unambiguous”.
- Requests for consent must be “clearly distinguishable from the other matters” and presented in “clear and plain language”
- Data subjects can withdraw previously given consent whenever they want, and you have to honor their decision.
- Children under 13 years of age can only give consent with permission of their parents or legal guardian.
- You need to keep documentation of the consent.
If we follow the rules mentioned above and properly acquire consent, then recording patients is legal. Nevertheless, if you are interested in finding more about how to record, store and share videos in compliance with GDPR then please refer to this article.
Moreover, when it comes to the ethicality of recording patients, consent is also a necessary part of it. Nevertheless, we should consider other factors beyond obtaining a patient’s consent. For example, we should not record patients who are in a bad condition as they may not fully understand what they are consenting to.
If you record a patient you also have a legal and moral obligation to protect that video from unauthorized viewing. It is your obligation to implement privacy by design architecture in the system(s) you use for recording, sharing, and commenting.
Is it practical to record patients?
Now that we have covered the ethicality and legality of recording patients let us talk about the practicality. Recording patients can be a very practical tool for teaching. This allows students and trainees to go over the content afterwards. In turn, providing more opportunities for self-reflection as well as providing peer-to-peer feedback.
Moreover, unless recording super precise clinical procedures (like surgeries) for educational purposes, we don’t need advanced equipment to carry out recordings. When it comes to educating communicational skills, a simple smartphone or tablet camera will suffice to generate the required videos. However, we advise using an external microphone to ensure that the audio is well-recorded.
Nevertheless, there can still be an impractical element to patient recording. Even if patients have consented to being recorded, they may still feel uncomfortable and this could negatively affect their care. To avoid this, we must actively monitor for changes in the way patients interact after turning on the camera. If it seems that they are becoming uncomfortable or if their behavior suddenly changes then it may be best to turn off the recording.
What are the best practices for recording patients?
Before recording patients, we need to consider several privacy concerns. We should only use the recordings for educational purposes and restrict access to those who do not need to see it. Therefore, to ensure best practice, we recommend using an application that encrypts the video immediately as it is recorded. This ensures the privacy and security of the content in the video. For this, we recommend using the Videolab Recorder.
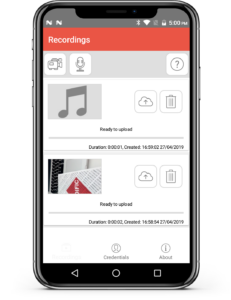
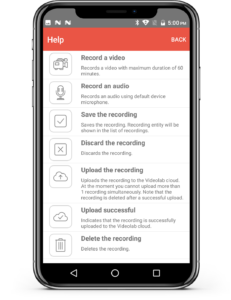
Additionally, we should only view recordings on a secure platform that ensures privacy and security. This platform should have the highest standard in security and privacy by design architecture. Moreover, it should comply with the regulations stated in the GDPR. That is of course why Videolab exists, Videolab is a secure online platform that allows you to record, upload, share and comment on videos, while keeping the highest standard in security and privacy by design architecture and complying with the GDPR. Thus, Videolab will deal with the privacy concerns of recording patients, allowing all efforts to be focused on using the recordings to educate trainees and students in the best way possible. Would you like to read about how leading university medical hospitals have implemented this? Check out the success story of Maastricht University here.
Would you like to begin recording? Or is it time to move your unsafe recordings to a safe system? Contact us!